(Solved): Case Study: Robert's Respiratory Distress Robert, a 68 -year-old male with a history of chronic obst ...
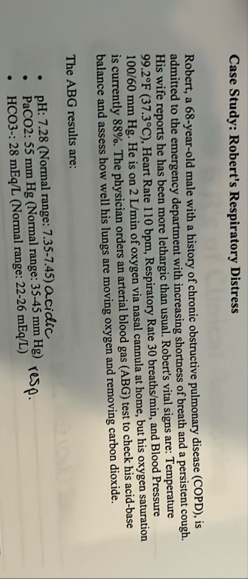
Case Study: Robert's Respiratory Distress Robert, a 68 -year-old male with a history of chronic obstructive pulmonary disease (COPD), is admitted to the emergency department with increasing shortness of breath and a persistent cough. His wife reports he has been more lethargic than usual. Robert's vital signs are: Temperature
99.2\deg F(37.3\deg C), Heart Rate 110 bpm , Respiratory Rate
30breath(s)/(m)in, and Blood Pressure
(100)/(60)mmHg. He is on
2(L)/(m)inof oxygen via nasal cannula at home, but his oxygen saturation is currently
88%. The physician orders an arterial blood gas (ABG) test to check his acid-base balance and assess how well his lungs are moving oxygen and removing carbon dioxide. The ABG results are: pH: 7.28 (Normal range: 7.35-7.45) acidic PaCO2: 55 mm Hg (Normal range:
35-45mmHg) HCO3-:
28mE(q)/(L)(Normal range:
22-26mE(q)/(L)) resp.